Alpha-1 antitrypsin deficiency
Vertex is focused on discovering, developing and producing innovative medicines so people with serious diseases can lead better lives. Our scientists don’t see the impossible as an obstacle; they see it as a good place to start.
Vertex is focused on discovering, developing and producing innovative medicines so people with serious diseases can lead better lives. Our scientists don’t see the impossible as an obstacle; they see it as a good place to start.
About alpha-1 antitrypsin deficiency (AATD)
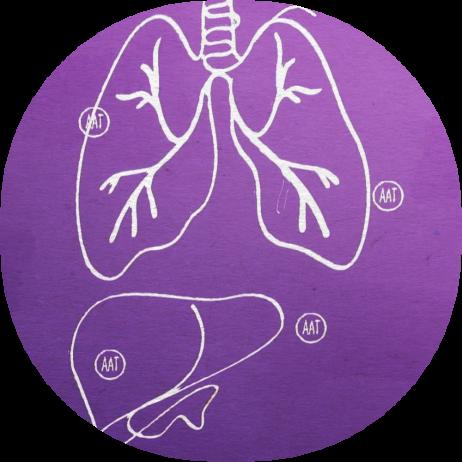
What is alpha-1 antitrypsin deficiency? AATD is an inherited disease that can cause damage to both the lungs and the liver. Many people with AATD primarily develop lung disease with symptoms such as wheezing or shortness of breath. These symptoms can worsen and progress to declining lung function and advanced lung disease, potentially requiring a lung transplant. The liver disease associated with AATD is often underrecognized, but it can also lead to severe damage. Liver problems can present at any time, or not at all, and can cause jaundice and swelling in the legs or other parts of the body. It can also progress to advanced liver disease like cirrhosis or liver cancer.
There is currently no cure for AATD. There are also no treatments that target the underlying cause of the disease or that address the liver disease associated with it. Current treatments are aimed at alleviating symptoms and reducing the progression of lung disease. Even with treatment, people living with AATD experience recurring hospital visits and a shortened life expectancy.
How is AATD diagnosed? AATD is often diagnosed with a blood test that shows low alpha-1 antitrypsin (AAT) levels. Genetic testing confirms the diagnosis and can identify the mutation. One of the biggest challenges with AATD is that many people don’t know they have it. People living with AATD may not be diagnosed until later in adulthood because it is often underdiagnosed or misdiagnosed as a different lung or liver disease.
What is the underlying cause of disease? AATD is caused by changes in the SERPINA1 gene that encodes the AAT protein. In the most common form of AATD, these changes to SERPINA1 cause the body to produce misfolded AAT protein that gets trapped inside the liver (where most AAT is made). This leads to low levels of AAT protein in the blood, preventing normal amounts of AAT from traveling to the lungs. Low blood levels of AAT can cause inflammation and damage to healthy tissues, especially in the lungs. The accumulation of defective AAT trapped in the liver is what leads to liver disease.
The Vertex approach
We’re focused on discovering and investigating medicines aimed at treating the underlying cause of AATD. Although severe AATD was discovered in 1963, and the misfolding defect seen in its most common variant was described over 20 years ago, there are still no treatments that address both the lung and liver manifestations of the disease. Building on our pioneering research with protein folding in cystic fibrosis, we’re developing potential medicines with the aim to treat people with AATD.
Our scientists are researching oral small molecules, with the goal to treat the underlying cause of disease and target both the lung and liver disease associated with the most common form of AATD. We’re currently investigating a portfolio of small molecules as potential medicines for the treatment of AATD.
Pipeline
These programs are investigating treatments or outcomes that have not received approval from a health authority. The information presented is not intended to convey conclusions of safety or efficacy. There is no guarantee that the outcome of these studies will result in approval by a health authority.