Cystic fibrosis
Vertex is focused on discovering, developing and producing innovative medicines so people with serious diseases can lead better lives. Our scientists don’t see the impossible as an obstacle; they see it as a good place to start.
Vertex is focused on discovering, developing and producing innovative medicines so people with serious diseases can lead better lives. Our scientists don’t see the impossible as an obstacle; they see it as a good place to start.
About cystic fibrosis (CF)
What is cystic fibrosis? CF is a rare, chronic and life-shortening genetic disease. It’s a progressive, multi-system disease that affects the lungs, liver, gastrointestinal tract, pancreas, sinuses, sweat glands and reproductive tract. In the lungs, this leads to the buildup of abnormally thick, sticky mucus that can cause chronic lung infections and inflammation, resulting in progressive lung damage and premature death in many people with CF. Other complications can include malabsorption and failure to thrive due to pancreatic disease, diabetes, liver disease, bone disease or osteoporosis, depression and anxiety. The median age of death is in the 30s, but with treatment, projected survival is improving.
People with CF require a combination of treatments that address problems in their lungs, digestive system and other parts of their body. They are living longer as a result of earlier diagnosis through newborn screening and improved care. However, there’s still a significant burden for people with this disease and their families associated with treatment and regular monitoring (often through regular visits to a hospital or CF care center).
How is CF diagnosed? CF can be diagnosed through newborn screening programs or during the first few years of life. Many newborns are screened with a blood test (heel prick) taken soon after a baby is born. The diagnosis is confirmed with a sweat test. Genetic testing can identify the mutations.
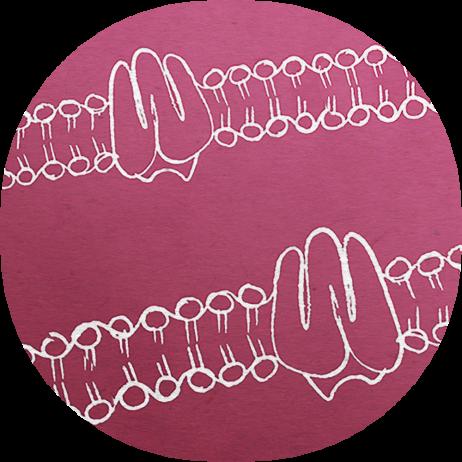
What is the underlying cause of disease? CF is caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene, which result in a defect and/or reduction in the amount of CFTR protein that the body makes. Children must inherit two defective CFTR genes — one from each parent — to have CF. While there are many different types of CFTR mutations that can cause the disease, the vast majority of all people with CF have at least one F508del mutation. The defective or missing CFTR protein results in poor flow of salt and water into or out of the cells in a number of organs, including the lungs. This leads to the buildup of abnormally thick, sticky mucus that can cause chronic lung infections and progressive damage to the lungs.
The Vertex approach
We have spent more than 20 years doing what was once thought impossible — discovering, researching and developing medicines to treat the underlying cause of CF. When we started our work in CF, the proof of concept that a small molecule could address a mis-folded or “broken” protein had not yet been tested.
Our portfolio approach focuses on bringing multiple compounds into clinical studies and using clinical data to inform drug discovery and development. The work starts in the lab with the design, synthesis and testing of tens of thousands of compounds. Only the most promising potential medicines then move into clinical trials.
There are two unique mechanisms of action in all four of our combination CFTR modulator medicines: (1) Correctors (lumacaftor, tezacaftor, elexacaftor, vanzacaftor) are designed to increase the amount of CFTR protein at the cell surface by facilitating the processing and trafficking of the CFTR protein. (2) Potentiators (ivacaftor and deuterated ivacaftor) are designed to increase the channel open probability of the CFTR protein delivered to the cell surface to improve the flow of salt and water across the cell membrane.
Vertex advanced the first of these potential medicines into clinical development in 2006. Since then, four innovative medicines have been approved and are available to certain eligible people with CF, and our research is ongoing as we continue to discover and develop medicines for potentially all people with CF.
We have set a high bar for ourselves but have not stopped our efforts to discover and test additional medicines and combination therapies. We’re also investigating potential treatments for people with CF who do not make any CFTR protein at all. We are investing in our own science and with our external partners, Arbor Biotechnologies, CRISPR Therapeutics and Moderna, Inc., to develop other potential approaches to treat the approximately 10% of people who are not expected to respond to CFTR modulator medicines. Our efforts to discover and develop therapies to potentially reach all people with CF through alternative investigational technologies have been underway for years, including messenger ribonucleic acid (mRNA) and gene editing. We remain relentless in our pursuit to finding treatments for all people living with CF.
Pipeline
These programs are investigating treatments or outcomes that have not all received approval from a health authority. The information presented is not intended to convey conclusions of safety or efficacy. There is no guarantee that the outcome of these studies will result in approval by a health authority.